The incidence of alcohol-related liver disease is decreasing but not rapidly enough. In Denmark, about twice as many people die from alcohol-related cirrhosis per capita as in Sweden and Norway. More systematic detection and treatment could prolong and improve many lives. If such a poor prognosis were related to cancer, there would definitely be greater awareness and an action plan, but liver disease has a low profile in the media.
Harmful alcohol consumption is by definition harmful for several organs and has negative social and economic effects. The latter deserves several separate articles. The focus here is only on how alcohol damages the liver, because alcohol is the most common cause of liver disease in Denmark.
Alcohol-related liver disease includes fatty liver disease, hepatitis and cirrhosis. Fatty liver disease can disappear again and has no symptoms. Hepatitis is rare; it causes jaundice and often severe symptoms that lead to hospitalization, but it can also disappear again. Cirrhosis is the alcohol-related liver disease that clearly requires the most hospital resources.
We are doing better
In cirrhosis, so much scar tissue has formed that the liver cannot become completely normal again. Alcohol causes about 80% of the cirrhosis cases in Denmark. People with cirrhosis caused by alcohol have an appalling prognosis in Denmark; they are typically in their late fifties when diagnosed, but despite their relatively young age, few are alive 5 years later.
Fortunately, the number of new cases of alcohol-related liver disease has declined in Denmark in recent years. The best explanation is the fact that the baby boomers consumed more alcohol throughout their life than later generations. As these baby boomers approached 60 years in the early 2000s, the incidence of alcohol-related liver disease in Denmark peaked.
Now a more moderate generation is approaching 60 years, and this means that fewer people are diagnosed with alcohol-related liver disease now than in 2010. This is good news. In addition, it is gratifying that we expect these numbers to continue their decline.
Over the years, we have become better at treating the complications associated with cirrhosis, and survival has increased slightly. That is fine, but there is still room for improvement. For example, the number of people dying from cirrhosis per capita is about twice as high in Denmark as in Sweden and Norway.
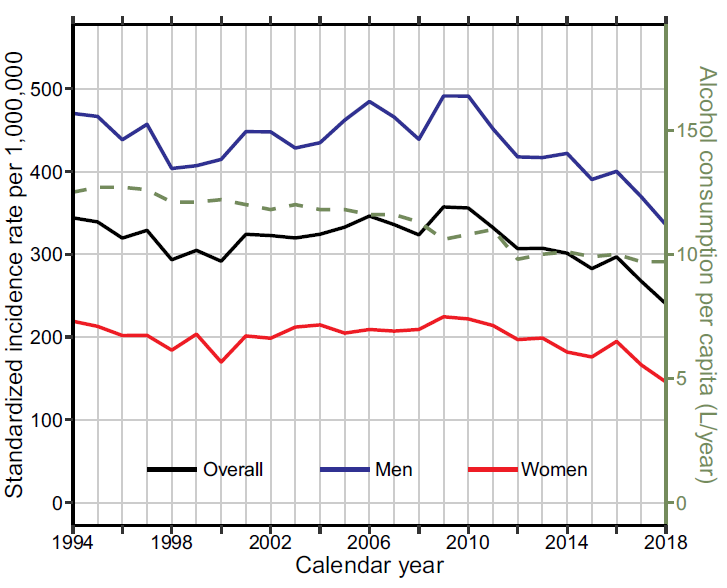
Annual incidence rate of alcohol-related liver disease in Denmark. The dashed line shows the annual per capita consumption of alcohol for adults.
We have the tools
Improvements have been achieved, and they can continue with various types of preventive measures.
Primary prevention includes measures to prevent alcohol-related liver disease from occurring. Structural measures such as raising the price of alcohol and restricting access can be deployed, and individual-based measures can also reduce alcohol intake among people who have not yet developed liver disease. Probably the most effective change in recent decades has been in the way individual people think about alcohol.
I cannot speak for everyone, but I have a clear impression that there used to be more people who thought that driving with a little too much alcohol in the blood was okay. Drinking alcohol on the job was also more widely accepted. These changes in attitudes toward alcohol have presumably contributed to the decline in the incidence of alcohol-related liver disease.
Secondary prevention means early detection of alcohol-related liver disease. In recent years, tools have been developed that can tell relatively easily how much scar tissue a person with harmful alcohol consumption has developed in the liver. A large amount of scar tissue means that cirrhosis has developed. So we have tools that can be used to screen for alcohol-related liver disease, and we hope that we can diagnose alcohol-related liver disease earlier than we typically do now.
The vision is that earlier initiatives will enable us to more optimally help people with both their alcohol dependence and their liver disease. If this is successful, these people will probably live both longer and have a better quality of life, and studies are underway to investigate this. I hope that we will achieve collaboration between general practitioners and hospitals in a few years, so that the general practitioners can carry out the screening in their practices with a simple blood test. The screening can then result in offering treatment for alcohol dependence and/or further investigation of and treatment for liver disease.
Low-hanging fruit
Tertiary prevention means treating people with liver disease and often — although not always – their alcohol dependence. Treating alcohol dependence is predominantly a municipal task in Denmark and is managed differently in each municipality. My experience is that people often get lost along the way from the hospital to the municipal treatment centre, and I think some low-hanging fruit can be harvested by relocating part of the municipal alcohol counselling service to the hospital setting.
Treating people for cirrhosis mainly includes nutrition and preventing and treating the complications that can occur. We do not yet have treatment that can remove the scar tissue in the liver, but we can often give these people a well-meaning, beneficial push towards being liberated from alcohol and improving their diet, and then we can provide medication to deal with any complications.
The trend is therefore heading in the right direction: fewer people newly diagnosed with liver disease and better treatments for those who do have liver disease.
Alcohol has a low profile
The reason why I am not satisfied with the current trend is that we are still not doing enough to help people with alcohol problems with or without concomitant liver disease. I am convinced that we could prolong and improve many people’s lives by more systematically detecting and treating their alcohol problems.
I am also convinced that alcohol-related liver disease has an excessively low profile in the media – if it were cancer that led to such a poor prognosis, there would certainly be greater attention and an action plan by the health authorities.
At the hospitals, we can also do more to improve the treatment of people with alcohol-related liver disease. There are far fewer clinical trials per death from alcohol-related liver disease than there are for other liver diseases.
All in all, politicians, municipalities, administrative regions, general practitioners, foundation boards, journalists and society as a whole should all pay far more attention to alcohol and its many sad effects. Their attention could contribute to a continued reduction in the number of people dying from alcohol-related liver disease.
Figure 1. Annual incidence rate of alcohol-related liver disease in Denmark. The dashed line shows the annual per capita consumption of alcohol for adults.
