Diabetes was first described more than three millennia ago on Egyptian papyrus scrolls, so it has probably always plagued humanity. However, Anette-Gabriele Ziegler, one of the world’s leading clinical researchers on type 1 diabetes, thinks that this could soon end. Her development of innovative screening programmes has created pioneering new knowledge about the cause and can now pave the way for better prevention, earlier diagnosis and therapy aiming for a future world without type 1 diabetes. Anette-Gabriele Ziegler is receiving the EASD–Novo Nordisk Foundation Diabetes Prize for Excellence for her efforts to understand, prevent and combat type 1 diabetes.
Most people associate old age with illness. The body deteriorates physically. The delicate balance of cells shifts. The immune system is weakened and overcome more easily. Nevertheless, some diseases strike at the opposite end of the age spectrum. They affect children because the immune system overreacts with youthful vigour and destroys some of the systems intended to help us live a long life.
Type 1 diabetes is one such autoimmune disease. It destroys the beta cells of the pancreas, stopping the production of insulin, a hormone that ensures that sugar in the blood can be stored as energy in muscles, liver and fat. Scientists have been trying to understand why and how this happens.
What we have found is that as soon as we can detect more than one autoantibody in a child, this means the clock has started to type 1 diabetes, and there is no way of return except if we can develop therapies that can delay the onset or can reduce the speed. So my research has very much focused on the factors that are important to start the clock and how we can prevent it from starting in the first place.
A chronic autoimmune disease
With one of the greatest discoveries in medical history, the insulin era of type 1 diabetes started a little more than a century ago, when surgeon Frederick Banting and student Charles Best at the University of Toronto treated a 14-year-old dying from diabetes with an injection of the hormone. The horror of the life-threatening disease had been taken away.
“My uncle was born the year Banting and Best began their experiments. At age 21, in the military, he was diagnosed with type 1 diabetes. This saved him from the war, and insulin saved his life, but he died from diabetic complications already at age 55. Today people with diabetes live longer, but conventional insulin therapy is by its very nature a treatment that regulates their lives day and night, year in and year out. My vison is to create a world without type 1 diabetes,” explains Anette-Gabriele Ziegler, Professor and Director of the IDF Institute of Diabetes Research, Helmholtz Zentrum München, German Research Center for Environmental Health.
Together with his friend Hellmut Mehnert, who later became Anette-Gabriele Ziegler’s teacher and mentor, her uncle scripted a play Better than Insulin. This inspired her to the groundbreaking advances in insulin treatment and to a lifelong quest to understand and battle type 1 diabetes. She began her medical studies in Munich in 1978 and received her licence to practice medicine in 1984 and a doctorate two years later with a dissertation on cellular immune phenomena in the manifestation of type 1 diabetes.
A research grant then took her to the Joslin Diabetes Center at Harvard University in Boston, where she joined diabetes pioneer George S. Eisenbarth, who was the first to define type 1 diabetes as a chronic autoimmune disease.
Already in the 1950s it had been demonstrated that insulin antibodies form days to weeks after the start of insulin treatment. But it was not until the early 1980s that researchers discovered the presence of antibodies to insulin already before the first insulin injection.
Antibodies predictive of future diabetes
The body’s natural defence system, the immune system, mistakes the body’s own cells as foreign cells. In type 1 diabetes, the beta cells in the pancreas are destroyed and, along with them, the insulin production.
My stay at Joslin gave me the opportunity to work with both Eisenbarth and his colleague Stuart Soeldner and really inspired me to work on autoimmunity to understand how type 1 occurs.
Using radiolabelled antigens, Stuart Soeldner developed an assay that became the gold standard to detect and quantify the autoantibodies. With this test, Anette-Gabriele Ziegler started measuring autoantibodies in a collection of samples from the first-degree relatives of people with type 1 diabetes from the Joslin Family Study collection of samples as well as from her home country, Germany.
“It was this work that made me realise that the autoantibodies created by the body itself were predictive of future type 1 diabetes. The antibodies were present in many younger children who later developed type 1 diabetes. Insulin was now not only the saviour of type 1 diabetes. Its presence also appeared to be an important autoimmune target – a main reason why the disease developed.”
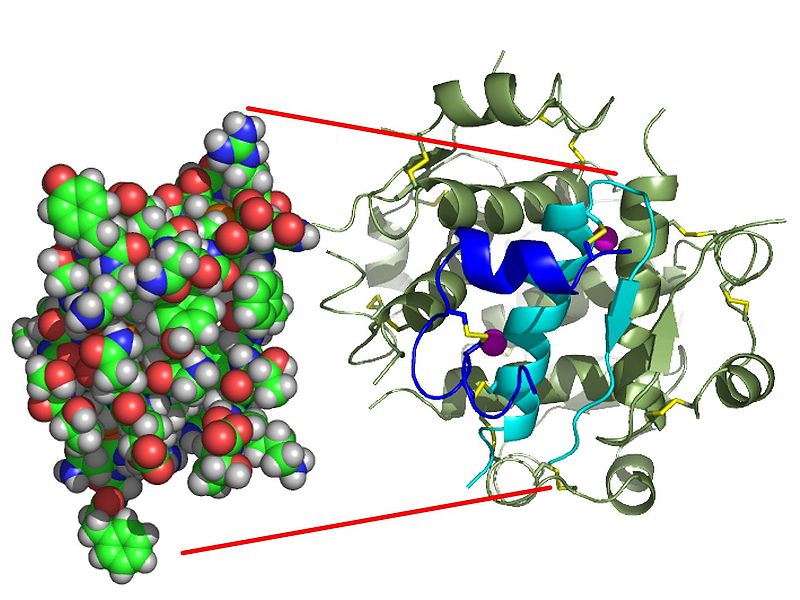
The structure of insulin. Credit: Isaac Yonemoto
Insulin is the original target
Anette-Gabriele Ziegler returned to Germany in 1988 with the novel idea of conducting a study enrolling genetically susceptible children at birth to understand how and among whom type 1 diabetes manifests clinically. The BABYDIAB study became the world’s first prospective diabetes birth cohort following the children at regular intervals throughout childhood and adolescence.
“This provided an important tool to understand susceptibility to developing autoimmunity and type 1 diabetes at a very early stage in the first 2 years of life and to find biomarkers for diagnosis regardless of symptoms,” says Anette-Gabriele Ziegler.
Over the next decade, this pioneering study of how children naturally develop type 1 diabetes led to several groundbreaking discoveries, such as insulin being the original target of autoantibodies and autoimmunity starting in the first three years of life among children developing type 1 diabetes. The earlier it starts, the faster was the progression to clinical disease.
“Importantly, insulin autoantibodies – or IAAs – were always present already in the age 9-month samples, and thus insulin appeared to be a critical immune target of the disease.”
Longest-running from birth natural history
However, an Australian-Italian colleague, Ezio Bonifacio, working at the Middlesex School of Medicine in London and who later became her husband, was not so convinced. He believed that other islet cell autoantibodies – ICAs – were equally important. These also appear long before the clinical onset of type 1 diabetes, and more and more of these autoantibody targets were detected during the 1990s.
We started working together and, with other colleagues, we sought to find out more about these antibodies.
In particular, a pathbreaking collaboration of the three longest-running from birth natural history studies led to landmark results and had a transforming impact on the diagnosis of type 1 diabetes.
“We found that the first early peak of autoimmunity is linked to insulin autoimmunity but that the presence of multiple islet autoantibodies constitutes the critical point of no return for type 1 diabetes to develop. But the message remained the same. The antibodies against insulin were the first,” explains Anette-Gabriele Ziegler.
Stopping the unstoppable clock
When Anette Ziegler left the lab of her mentor George Eisenbarth in the late 1980s, he had given her a clock as a gift. Now 20 years later, he was ill.
“I wrote him an e-mail saying: I still have your gift in my office, and I just changed the battery. This clock is still working. And he replied: similar to this clock, I'm still enjoying working. But I knew that there was something different behind his words. We all knew that probably he would not carry on working for long.”
Because they were writing the paper about 20 years of research, the metaphor of the clock became part of it.
“And then we all sort of defined it as the clock to type 1 diabetes that starts when these multiple antibodies develop. Ever since, our goal has been to find ways to slow down or stop this unstoppable clock.”
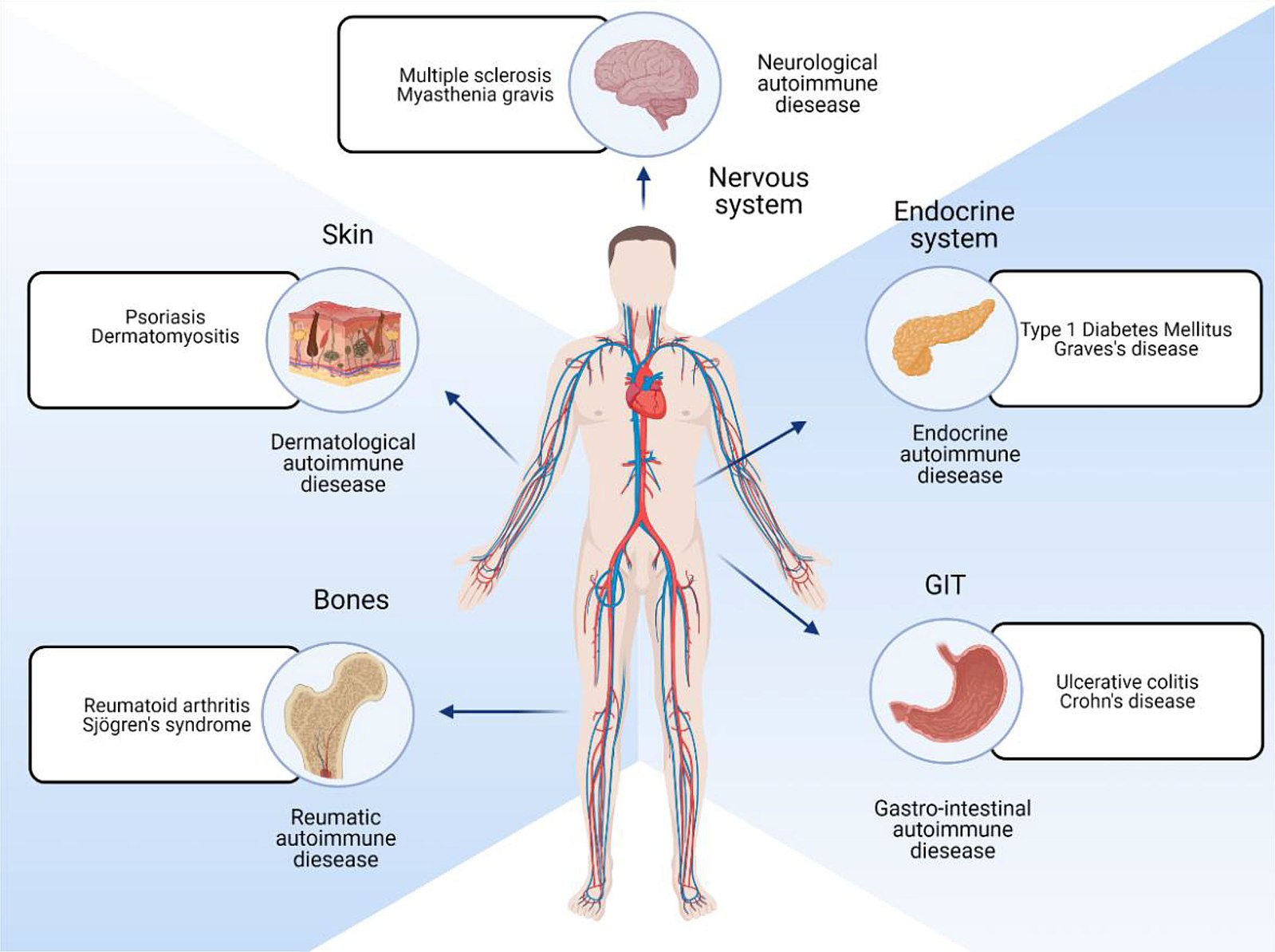
Different locations of the body that are affected by autoimmune diseases. Credit: Katie Glover, Deepakkumar Mishra, and Thakur Raghu Raj Singh
Insulin as a protector against disease
Similar to other autoimmune diseases and allergic reactions, the aggressor in type 1 diabetes is the immune system. Based on their previous findings, Anette-Gabriele Ziegler and colleagues thought they might somehow be able to suppress or re-educate the immune system to save the beta cells from destruction.
“Since we knew that the very first autoantibodies develop against insulin, we wondered whether we could create tolerance by stimulating children at high risk very early with small amounts of insulin – before they even turned 1 year old,” says Anette-Gabriele Ziegler.
She therefore initiated pilot studies giving insulin subcutaneously or intravenously to people with autoantibodies against insulin – with promising results. Changes in the immune system were registered and suggested a delay in the progression of the disease. However, when larger trials were performed, the effect could not be seen.
“Were we wrong to consider insulin as a primary antigen, or did we choose the wrong re-education method? Our concern was that it may be too late to give the therapy after the insulin autoantibodies develop, so we tried again with children before they developed the autoantibodies.”
In Pre-POINT, a clinical pilot study in Germany, Austria and the United States, the researchers identified a dose of oral insulin that was both safe before 1 year of age and triggered an immune response that could produce tolerance.
“We measured increased T- and/or B-cell immune response to insulin that differed markedly from the typical responses of children who develop diabetes. This was very encouraging – that giving insulin in fixed small doses was safe but also that it seems to promote tolerance in children and hopefully prevents them from developing diabetes,” explains Anette-Gabriele Ziegler.
Preventing and improving
In 2015 Anette Ziegler was ready for the next big step – the Fr1da study that offers screening for autoantibodies to all children between 2 and 10 years old throughout Bavaria, Germany.
“We now knew that type 1 diabetes can be diagnosed early by detecting the autoantibodies. But we wanted to determine whether screening for type 1 diabetes is feasible – not just among children who have a relative with type 1 but in a population,” explains Anette-Gabriele Ziegler.
Another aim was to learn how to prevent the serious metabolic changes connected with the development of type 1 diabetes, especially to improve the quality of life and to reduce the stress diabetes causes through preventive education and outreach. With more than 150,000 children screened so far, the Fr1da study has shown that type 1 diabetes can be diagnosed early in an entire population.
“This can help to prevent diabetic ketoacidosis – a serious, life-threatening complication that can arise if the disease is recognised too late – and to improve clinical care and especially provide a way to actively recruit children at high risk for subsequent preventive measures,” she adds.
Genetic testing identifies newborns at risk
The culmination of more than 25 years of dedicated effort first came in 2015 when Anette-Gabriele Ziegler helped launch the Global Platform for the Prevention of Autoimmune Diabetes (GPPAD), which brought together academic research institutions and hospitals across Europe. The goal was to establish an international research infrastructure dedicated to preventing the development of type 1 diabetes.
“The initiative focuses on preventing the autoimmunity that precedes and destroys the beta cells that produce insulin. GPPAD carries out newborn screening in the general population to identify infants at high genetic risk of developing type 1 diabetes and to offer them participation in trials to prevent disease initiation. This is the first initiative to target the general population with a polygenic risk score for type 1 diabetes,” says Anette-Gabriele Ziegler.
The ultimate goal is to expand the screening initiatives to include other states in Germany and other European countries. Led by Anette-Gabriele Ziegler, GPPAD is one of the few major primary prevention platforms in the world that will strongly influence children’s health and open up new ways to prevent several other diseases.
“We now have such good understanding of the timing of autoantibodies and the genetic contribution to their development that we have developed a genetic risk score that is used to screen newborns for type 1 diabetes to enable early diagnosis of the risk of developing the disease,” explains Anette-Gabriele Ziegler.

Anette-Gabriele Ziegler has created pioneering new knowledge through numerous innovative screening programmes. Credit: EASD.
Might only be part of the solution
With simple genetic testing, researchers can identify newborns who have a 1 in 10 risk of developing the early signs of type 1 diabetes compared with the general population’s risk of 1 in 250. GPPAD screening has so far identified more than 3,500 newborns with an increased genetic risk based on their genetic scores.
“Of these, 1,050 infants have been enrolled in pan-European GPPAD-POInT (Primary Oral Insulin Trial), with the aim of preventing the destruction of the insulin-producing beta cells in the pancreas among children at increased risk of type 1 diabetes and therefore preventing the disease from developing,” says Anette-Gabriele Ziegler.
In this connection, Anette-Gabriele Ziegler’s institution Helmholtz Zentrum München and the Technical University of Munich have been instrumental in advancing the research.
“Helmholtz means a lot to me because it introduced me to diabetes research at another level, another generation of research with many new technologies and genomic tools that help me with analysis, but it has also been instrumental in translating the research into new treatments that can benefit society,” adds Anette-Gabriele Ziegler.
Although the use of oral insulin to re-educate the immune system seems promising among children, there are still some challenges to be solved. Insulin might become less relevant as a driving antigen as the disease progresses and with increasing age while other islet cell antigens become more prominent.
“For these reasons, novel and other forms of antigen-specific immunotherapy are very much welcomed.”
A world without 1
Although the incidence of type 1 diabetes among young children is still steadily increasing and it is the most common metabolic disease in childhood and adolescence, Anette-Gabriele Ziegler believes that today, unlike 30 years ago, there are great hopes for a world without type 1 diabetes.
So I think really, we are steps ahead compared to 20 years ago. We have really promising treatments undergoing clinical trials that may be able to prevent the clock from starting or to slow down the clock, and above all, our understanding of the disease and ability to diagnose it in time have improved greatly.
However, bridging the gap between basic science and clinical practice has not always been easy.
“I felt that doing research as a doctor and not doing basic research in a research institute always somehow made you feel between chairs. But I must say, I also like that challenge. I even like the challenge of running back and forth between the intensive care ward and my lab, or between caring about patients and having a paper rejected. This polar thing: I think this also pushed me rather so I didn't really suffer from it.”
Things that sound impossible
There are still many unknown factors in understanding how the complex genetic elements and environmental factors interact and whether this is all initiated by viral infections, dysfunction in the microbiome or something else,” says Anette-Gabriele Ziegler.
However, Anette-Gabriele Ziegler hopes that the newly developed methods for screening newborns and children can be expanded globally, so that parents, through training, can be prepared for type 1 diabetes and thereby optimise treatment.
“My vision and goal, as it was three decades ago, is a world without type 1 diabetes. I get stimulated by people, by ideas, by new things, and I still want to discover new things. I like things that sound impossible but become possible. I'm a doctor, and I've worked with many, many people who have type 1 diabetes. I help them and I know what it means to have that disease 24 hours every day, so I would be extremely happy to know that one day maybe we have really cured this disease, so that children never again need to inject insulin,” concludes Anette-Gabriele Ziegler.
