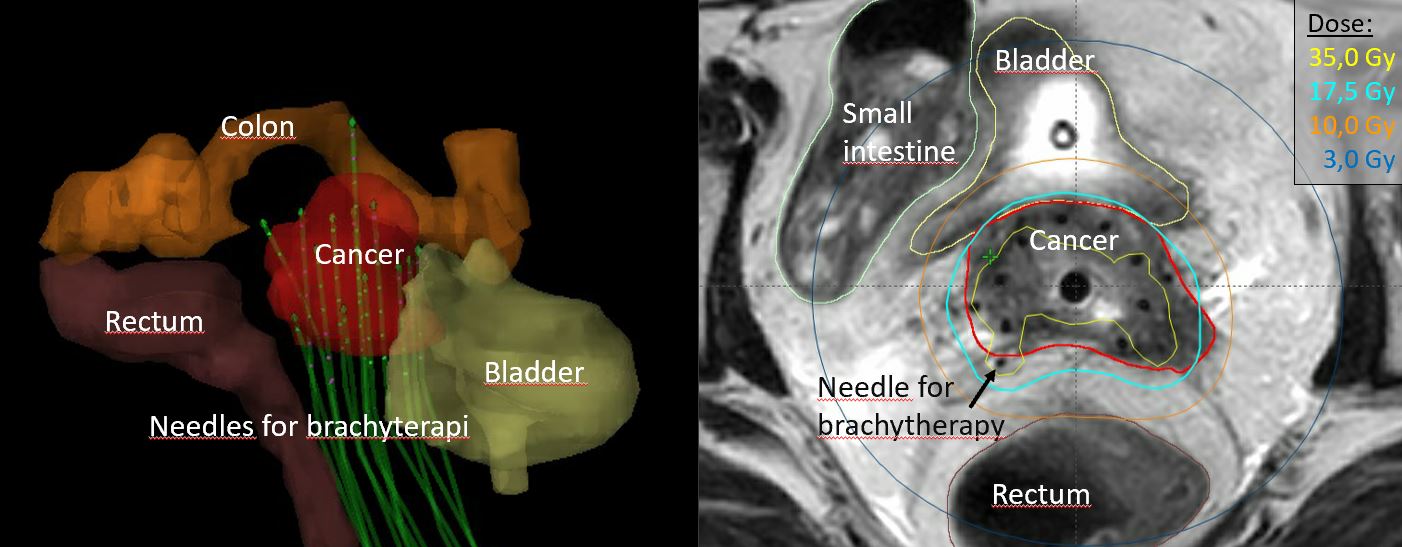
Brachytherapy (internal radiation therapy), which uses a radiation source sealed in an implant, is key in cervical cancer treatment. Precision is therefore crucial for controlling the disease and for avoiding unnecessary side-effects. The precision was previously based on X-rays in two dimensions. Today, brachytherapy is guided using 3D magnetic resonance imaging (MRI). A new study shows that brachytherapy eliminates more than 90% of tumours, even very advanced ones. The next step is to avoid metastasis.
Every year, almost 600,000 women worldwide develop cervical cancer, with the highest frequency in low-income countries. Despite HPV vaccination programmes, Denmark still has about 400 cases per year, about half of which can be treated by surgery. Radiation therapy is the treatment of choice for the rest. A new study (EMBRACE I) shows that 3D MRI-guided adaptive brachytherapy could save thousands of lives worldwide each year and limit radiation-related side-effects.
“The study shows that treating cervical tumours differs greatly between 3D MRI scans and 2D X-rays. The exact location of the strong radiation source is absolutely crucial. However, we think that 3D MRI-guided adaptive brachytherapy is not yet being given sufficient priority, even in high-income countries, many of which do not yet have the equipment and training to carry out this state-of-the-art treatment, although MRI or at least CT scans are available in principle. We hope that our results can reveal how many lives can be saved and improved in a relatively simple and affordable way,” explain consultants Jacob Lindegaard and Lars Fokdal, Department of Oncology, Aarhus University Hospital.
Precision is crucial
Brachytherapy has been around for more than a century. Pierre Curie suggested that inserting a radiation source into a tumour would cause it to shrink. This method therefore enabled the delivery of a high dose of radiation to a tumour site, which might otherwise be difficult to access, such as in cervical cancer. He was right, but for half a century the treatment was considered too dangerous – both for patients and the clinicians who administered it.
“New types of radiation sources, shielding them and developing computer control have made brachytherapy safer for many types of cancer. Nevertheless, until about year 2000, only X-ray imaging was available, and this did not provide the necessary precision, which undoubtedly resulted in unnecessary side-effects and a greater risk of simply not targeting the tumour precisely,” explains Kari Tanderup, Professor, Department of Oncology, Aarhus University Hospital and Department of Clinical Medicine, Aarhus University.
With the development of computed tomography (CT) scanning technology, 3D X-rays became available. However, the development of MR scanning enabled clinicians more clearly to differentiate between cancerous tissue and the surrounding healthy tissues, which are adjacent. This meant that the radiation source could be positioned far more accurately. In 2000, the new opportunities led to the establishment of an international working group, the GEC-ESTRO GYN Working Group, which would actively support and shape the development of gynaecological brachytherapy.
“The Working Group aimed to identify a common language and standards for MRI-guided adaptive brachytherapy for cervical cancer treatment and to contribute to disseminating the technology to as many institutions as possible. When EMBRACE I was initiated we were 24, but today there are over 40 branches in the network in Europe, the United States and Asia, and with the convincing recent results, we hope and believe that the technology will become widespread in many more places around the world,” says Kari Tanderup.
Very cost-effective
Introducing MRI-guided adaptive brachytherapy has significantly improved long-term survival across all stages of locally advanced cervical cancer. A few years ago, one in three people died within 5 years of diagnosis. Today the figure is one in five, and a major reason for this improvement is undoubtedly that MRI-guided adaptive brachytherapy has contributed to the complete elimination of 92–95% of cervical tumours.
“The progression from X-ray to CT scanning – from 2D to 3D – was significant, but our new study shows that the progression from CT to MRI scanning further improves the treatment. Therefore, we hope that the results of the EMBRACE I study of more than 1300 people treated with MRI-guided adaptive brachytherapy recently published in Lancet Oncology may convince many more people that this technology should be given priority. MRI-guided adaptive brachytherapy is actually very cost-effective compared with other types of cancer treatment with significantly less therapeutic potential,” says Jacob Lindegaard.
According to the researchers, the financial investment in equipment is not necessarily enough to deter hospitals around the world from introducing MRI-guided adaptive brachytherapy. Instead, training qualified personnel is often the challenge. The technique of accurately positioning the radiation source and especially interpreting the images afterwards requires thorough training and experience.
“We are holding an increasing number of courses for physicians and oncologists from all over the world and, paradoxically, since the COVID-19 pandemic we have begun to reach a wider audience since we have had to hold the courses online. This naturally presents some challenges, but conversely many more people can afford to participate by saving on expensive travel,” explains Kari Tanderup.
You do not randomize who gets a parachute
Based on the potentially enormous clinical implications of the new study for the treatment of people with a deadly cancer, most people would probably think that a study like EMBRACE I would automatically feature in a leading journal in the field such as Lancet Oncology. However, the researchers were far from convinced, since this was not a randomized controlled trial with one group receiving treatment and one not.
“Our study was an observational study, in which everyone received the same treatment, instead of randomly choosing who should have the treatment and who is part of the control group. However, with a treatment like this, where availability of MRI is a straightforward advantage, this would obviously be difficult. You do not randomize who gets a parachute before jumping from a plane,” says Jacob Lindegaard.
In recent years, many journals have tended to publish more and more of this type of real-world data that summarize general practice, and in 2018 the United States Food & Drug Administration published a framework for its Real World Evidence Program for the same reason.
Combatting metastasis
Although the EMBRACE I study made major advances in treating locally advanced cervical cancer using MRI-guided adaptive brachytherapy, the researchers say that there is still much to do. EMBRACE II has therefore been started, drawing on the experience from EMBRACE I. The new research over the coming years on the side-effects among 1,500 women will focus especially on the external beam radiotherapy that precedes the insertion of the radiation source into the cervix.
“External radiation treatment is important for several reasons. This increases the radiation level up to about half of what is required, after which the brachytherapy selectively increases the radiation to a level at which the probability of the last cancer cell perishing becomes very high. Also, the external radiation serves to irradiate lymph nodes and the pelvic, inguinal or paraaortic region to which the cancer could otherwise spread,” explains Jacob Lindegaard.
Metastasis outside this region, to which the cancer can migrate from the primary tumour in the cervix, still presents the greatest challenge because this can often only be treated with chemotherapy.
“In recent years, immunotherapy trials have been conducted on groups of relapsing patients, even though the primary tumour has disappeared, but there has been no major breakthrough. However, we hope that immunotherapy as an adjunctive treatment following radiation therapy may be able to help reduce the risk of any recurrence. Nevertheless, clearly the first prerequisite for even attempting this is that women emerge from the treatment of the primary tumour as healthy as possible so they can tolerate further treatment. This why MRI-guided adaptive brachytherapy is so critical in this context,” concludes Kari Tanderup.
